Gout: Comprehensive Medical Overview & Clinical Guidance
*Introduction -
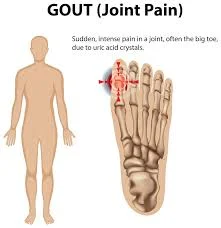
Gout is a chronic metabolic disorder characterized by the deposition of monosodium urate (MSU) crystals in joints and soft tissues, resulting from prolonged hyperuricemia. It is the most common form of inflammatory arthritis in adults and represents a significant burden on quality of life and healthcare systems. Gout is both treatable and preventable, yet it remains underdiagnosed and undertreated in many parts of the world.
---
Etiology and Risk Factors
1. Hyperuricemia
Hyperuricemia, defined as serum urate levels >6.8 mg/dL (the solubility limit of urate in plasma), is the fundamental biochemical abnormality in gout. Not all individuals with hyperuricemia develop gout, but virtually all patients with gout have hyperuricemia at some point.
2. Causes of Hyperuricemia
Hyperuricemia arises either from increased production or decreased excretion of uric acid.
A. Increased Production
High purine diet: Red meat, organ meats, shellfish
Increased cell turnover: Hematologic malignancies, psoriasis
Genetic disorders: Lesch-Nyhan syndrome (HGPRT deficiency)
Alcohol consumption: Especially beer (contains guanosine, a purine)
B. Decreased Excretion
Renal insufficiency
Medications: Diuretics (thiazides, loop), low-dose aspirin, cyclosporine
Genetic predisposition: Familial juvenile hyperuricemic nephropathy
---
Pathophysiology
Uric acid is the final product of purine metabolism. In humans, uricase (which converts uric acid to allantoin) is nonfunctional, leading to relatively high uric acid levels.
1. Supersaturation: When serum urate exceeds 6.8 mg/dL, it can crystallize.
2. Crystal deposition: MSU crystals deposit in cooler joints (e.g., big toe).
3. Inflammatory response: Crystals are phagocytosed by macrophages → activation of NLRP3 inflammasome → IL-1β release → neutrophil recruitment.
4. Clinical symptoms: The intense inflammatory response results in pain, erythema, swelling, and warmth.
---
Stages of Gout
Gout progresses through four clinical stages:
1. Asymptomatic Hyperuricemia
Elevated serum urate without clinical symptoms.
May last for years before first gout attack.
2. Acute Gouty Arthritis
Sudden onset of severe joint pain, swelling, redness.
Often monoarticular, commonly affecting the first metatarsophalangeal (MTP) joint.
Lasts 7–10 days if untreated.
3. Intercritical Gout
Asymptomatic interval between acute attacks.
MSU crystals still present in joints and tissues.
Duration shortens as disease progresses.
4. Chronic Tophaceous Gout
Seen in patients with prolonged uncontrolled hyperuricemia.
Characterized by tophi (chalky urate deposits), joint destruction, deformities, and chronic pain.
---
Clinical Manifestations
1. Articular Involvement
Podagra: First MTP joint (most classic presentation)
Other joints: Midfoot, ankle, knee, wrist, fingers, elbow (olecranon bursitis)
Onset: Typically nocturnal, maximal in 6–12 hours
Features: Extreme tenderness, redness, swelling, loss of function
2. Extra-articular Manifestations
Tophi: Subcutaneous urate deposits—firm, yellowish nodules on ears, fingers, elbows, knees
Renal involvement:
Uric acid nephrolithiasis
Chronic urate nephropathy
---
Diagnosis
1. Synovial Fluid Analysis
Gold standard
Needle aspiration of inflamed joint
Under polarized light microscopy: needle-shaped, negatively birefringent MSU crystals
Excludes septic arthritis (always consider in monoarthritis)
2. Laboratory Tests
Serum uric acid: Usually elevated but can be normal during acute flare
Elevated WBC count, ESR, CRP during acute attack
Renal function tests: baseline for ULT
3. Imaging
X-rays: Normal in early gout; chronic gout shows:
Punched-out erosions with overhanging edges (“rat bite”)
Tophi may be seen as soft tissue densities
Ultrasound:
“Double contour sign” (urate crystal layer on cartilage)
Dual-energy CT (DECT):
Detects urate crystals in joints and soft tissue (very sensitive)
---
Differential Diagnosis
Septic arthritis
Rheumatoid arthritis
Pseudogout (calcium pyrophosphate crystals; positively birefringent)
Psoriatic arthritis
Reactive arthritis
---
Management
A. Acute Attack Management
Goal: Rapid symptom relief and inflammation reduction
First-Line Options:
1. NSAIDs: Indomethacin, naproxen, ibuprofen
Contraindications: CKD, GI ulcers, heart failure
2. Colchicine: Best within 24–36 hours
Low-dose regimen (0.5 mg BID)
Side effects: GI upset, diarrhea
3. Glucocorticoids:
Oral prednisone or intra-articular triamcinolone
Preferred in renal impairment or NSAID intolerance
Adjunctive Measures:
Rest the affected joint
Ice application
Hydration
Avoid alcohol or purine-rich foods during flare
---
B. Urate-Lowering Therapy (ULT)
Indications:
≥ 2 attacks/year
Tophi or chronic gouty arthritis
Uric acid nephrolithiasis
CKD stage 2 or higher
Agents:
1. Xanthine Oxidase Inhibitors
Allopurinol:
Start low (100 mg/day), increase gradually
Max: 800 mg/day
Screen for HLA-B*5801 in Asians (risk of hypersensitivity)
Febuxostat:
Alternative for allopurinol-intolerant patients
Increased cardiovascular risk
2. Uricosuric Agents
Probenecid:
Enhances renal uric acid excretion
Not effective in renal impairment
3. Uricase Enzymes
Pegloticase: Converts uric acid to allantoin
For refractory, tophaceous gout
Treatment Goals:
Serum urate < 6.0 mg/dL (general goal)
< 5.0 mg/dL in patients with tophi
Prophylaxis During ULT Initiation:
Colchicine 0.5 mg daily or NSAID
Continue for 3–6 months to prevent flares
---
Lifestyle and Dietary Management
1. Diet
Avoid:
Organ meats (liver, kidney)
Shellfish, anchovies, sardines
Alcohol (esp. beer and spirits)
High-fructose corn syrup
Encourage:
Low-fat dairy products
Cherries (may reduce flares)
Vegetables, whole grains
2. Weight Loss
Reduces urate levels and flare frequency
3. Fluid Intake
Encourage ≥2 liters/day to prevent nephrolithiasis
4. Alcohol
Limit intake, especially beer and spirits
---
Complications
1. Articular Damage
Chronic inflammation → cartilage destruction → deformity, ankylosis
2. Tophi
Disfiguring, can ulcerate, become infected, or compress nerves/tendons
3. Renal Disease
Uric acid nephrolithiasis
Chronic urate nephropathy
4. Cardiovascular Risk
Associated with hypertension, dyslipidemia, stroke, MI
---
Gout in Special Populations
1. Women
Rare before menopause due to estrogen’s uricosuric effect
Post-menopausal women have increased risk
2. Elderly
Often atypical presentation (polyarticular, hand involvement)
More likely to have renal impairment affecting treatment options
3. Pediatric Gout
Rare, but seen in inborn errors of metabolism (Lesch-Nyhan)
---
Recent Advances
1. Imaging
DECT has revolutionized non-invasive diagnosis and monitoring of crystal burden.
2. New Therapies
Pegloticase and other recombinant uricases provide options for severe refractory gout.
3. Personalized Medicine
HLA-B*5801 screening to prevent allopurinol hypersensitivity in Asian populations
4. Comorbidity Management
Addressing metabolic syndrome, diabetes, and renal disease improves gout outcomes.
---
Prevention
Long-term serum urate control is key.
Educate patients about disease nature and lifelong management.
Adherence to ULT and lifestyle changes are crucial to prevent flares and complications.
---
Conclusion
Gout is a common and debilitating disease with well-understood mechanisms and effective treatments. While acute attacks are often dramatic and painful, long-term management with urate-lowering
therapy and lifestyle modification can prevent recurrence and joint damage. Early diagnosis, patient education, and individualized treatment plans are the cornerstones of successful gout management. With advances in diagnostics and therapy, the long-term prognosis of gout can be excellent if appropriately managed.



Comments
Post a Comment
“Thanks for joining the discussion! Please keep comments respectful and relevant. Spam or promotional links won’t be approved 😊”